

Body Mass Index (BMI) is a simple measure for weight-related health risk. It is one of the measures that your health care provider uses to determine your health risk in relation to your weight. It is a signal to your doctor to take a closer look and have a more detailed conversation with you about your health. The measure is used for adults aged 20 and older. The similar measure for children and teens is called BMI-for-age, or BMI percentile. This measure accounts for the child's sex and age, as well as their weight.
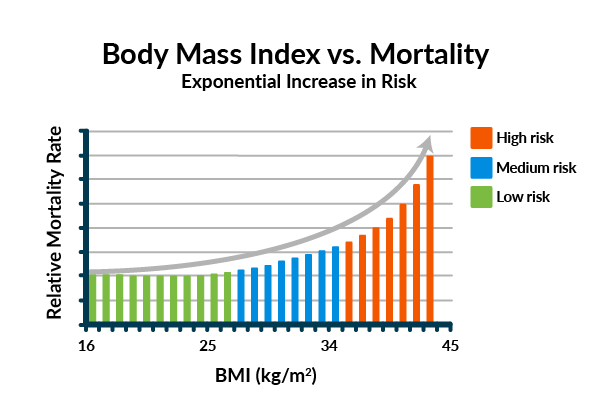
As recognized by global health organizations such as the US Centers for Disease Control and Prevention and the World Health Organization, BMI represents the relationship between weight and height to estimate the amount of fat in the body.1 A higher percentage of body fat is proven to be associated with increased risk for developing certain diseases such as heart disease, high blood pressure, type 2 diabetes, breathing problems, certain cancers, and death.2, 3, 4
How is BMI calculated?
Calculating your BMI is as simple as plugging your height and weight into an online BMI calculator for women and men, such as the one hosted by the US National Heart, Lung, and Blood Institute.
BMI formula: your weight (in kilograms) divided by your height squared (in meters), expressed as kg/m2.
- Formula: Weight (kg)/[height (m)]2
- Example: weight =92 kg and height= 1.78 m
- Calculation: 92/ (1.78)2= 92/3.17=29.0
However, it can also be calculated using the English System: your weight (in pounds) divided by your height squared (in inches) multiplied by 703.
- Formula: [Weight (lb)/height (in)]2 x 703
- Example: weight =202.8 lb and height= 70 in
- Calculation: [202.8/ (70)2] x 703= [202.8/4900] x 703= 29.1
BMI is interpreted by using the following weight categories.1
BMI (kg/m)2 | Weight Range | |
|---|---|---|
< 18.5 | Underweight | |
18.5-24.9 | Healthy Weight | |
25.0-29.9 | Overweight | |
30.0 or higher | Obese |
Overweight and obese are the ranges of weight that are greater than what is generally considered healthy for a given height, and are used as a signal for higher risk for certain diseases such as type 2 diabetes and obstructive sleep apnea.4 Underweight is the range of weight that is lower than what is generally considered healthy for a given height, and may indicate underlying medical conditions or an eating disorder and higher risk for conditions such as osteoporosis.
Why use BMI?
We know that BMI is not a perfect measure of health. Some of the known limitations include:
- It does not directly assess body fat and there are other measures such as waist circumference or DEXA scans that may be a better measure of body composition.
- It is not as accurate for athletes as it may not accurately assess body composition (read: does not take into account the weight of bones, muscles, or organs).5
- It is not as accurate for certain racial/ethnic groups such as those of Asian descent (the weight categories have different cut points for those of Asian descent; for example, overweight is defined as a BMI of 23.0-27.5 instead of 25.0-29.9 for those of non-Asian descent).6
- People with a similar BMI can have very different health risks due to genetics, lifestyle, and their environment.7, 8, 9
- Body fatness levels differ across demographic categories, and two people of the same BMI can have different levels of body fatness. For example, we know that women tend to have more body fat than men, older people tend to have more body fat than younger adults, and athletes tend to have less body fat than nonathletes.10
All of that being true, BMI continues to be the best estimation of weight-related health risk at a population level because of its scalability and accessibility—it is a simple calculation, it is based on easily measured values (height and weight), and it is relatively easy to understand.11, 15 Additionally, research has shown that BMI is strongly correlated with the gold-standard (read: best) methods for measuring body fatness.1, 12 Other measures of body composition, such as bioelectrical impedance, dual energy x-ray absorptiometry, skinfold thickness measurements, and underwater weighing, tend to be expensive, invasive, difficult to obtain, and require highly trained clinicians.15
Are there times when BMI is not the best measure?
For the people who regularly engage in vigorous activities or athletes, other measures of body composition may be more useful than BMI to assess their health risk associated with their weight, such as body measurements (waist, hip, arm, thigh) or skinfold thickness with calipers. Body measurements can be tricky to measure the same way each time, so it's best to have these measurements taken by a qualified health care professional.
BMI and the weight-loss journey
A BMI calculator for women and men, like the scale, is another tool that can be used to measure changes to your body composition and weight related health risks. When BMI is above the healthy range, scientific literature suggests that even modest decreases can significantly improve health by lowering the risk for high blood pressure, type 2 diabetes, heart disease, obesity-related cancers, and early death.13,14,15 Additionally, a weight loss of 5-10% has been associated with improvements in sleep quality, mood, and mobility.16,17 When BMI falls below 18.5, aiming to maintain a weight within the healthy range (18.5-24.9) may reduce the risk for health conditions associated with low body weight including osteoporosis.
Whether your goals are to lose weight, maintain your weight, or keep your weight steady in the healthy range, you’ll probably find that tracking the change in your weight (either in pounds or kilograms) is easier to interpret than changes in BMI. Understanding the BMI weight ranges, can help you connect your weight to potential health risks, however, BMI is just one measure of wellness. Most importantly, we recommend that you set goals, weight-related or otherwise, that will move you along the continuum toward a happier, healthier you.
1 Global Health Observatory. from http://www.who.int/gho/ncd/risk_factors/bmi_text/en/
2 Nguyen NT, Magno CP, Lane KT, et al. Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J Am Coll Surg. 2008;207(6):928-934.
3 Keum N, Greenwood DC, Lee DH, et al. Adult weight gain and adiposity-related cancers: a dose-response meta-analysis of prospective observational studies. J Natl Cancer Inst. 2015;107(2): djv088.
4 Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165(9):1217-1239.
5 Disability and Obesity. Centers for Disease Control and Prevention. from https://www.cdc.gov/ncbddd/disabilityandhealth/obesity.html
6 Chinese Community Health Resource Center. Body Mass Index (BMI) for adults. Retrieved on August 16, 2017 from http://www.cchrchealth.org/health-calculators/body-mass-index-bmi-adults
7 Faith MS, Kral, TVE. Social environmental and genetic influences on obesity and obesity-promoting behaviors: Fostering research integration. (2006). University of Pennsylvania School of Medicine.
8 Risk Factors. from https://www.nhlbi.nih.gov/health/health-topics/topics/obe/risks
9 NHLBI. 2013. Managing Overweight and Obesity in Adults: Systematic Evidence Review from the Obesity Expert Panel, 2013.
10 Gallagher D, et al.How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol. 1996; 143(3):228-39.
11 U.S. Preventive Services Task Force. Screening for obesity in adults: recommendations and rationale. Ann Intern Med. 2003 Dec. 2; 139 (11):930-2.
12 Flegal, KM, Graubard, BI.. Estimates of excess deaths associated with body mass index and other anthropometric variables. Am. J. Clin. Nutr., 2009. 89(4): 1213–1219.
13 Blackburn G. Effect of degree of weight loss on health benefits. Obes Res.1995;3(2):211s-216s.
14 Jensen MD, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation.
15 Wolin KY, Carson K, Coldotz GA.. Obesity and Cancer. Oncologist. 2010;15:556-565.
16 Alfaris N, et al. Effects of a 2-year behavioral weight loss intervention on sleep and mood in obese individuals treated in primary care practice. Obesity. 2015;23:558-564.
17 Vincent HK, et al. Obesity and weight loss in the treatment and prevention of osteoarthritis. PM R. 2012;4 (5 Suppl): S59-S67.
