The most important things to know about nutrition for diabetes
Included in this article:
How nutrition affects diabetes
There’s a reason so much of diabetes management focuses on diet: The food you eat directly drives your blood sugar levels. As your body breaks down what you eat, it turns any carbohydrates into simple sugars, which are then released into the bloodstream. Insulin, a hormone made by the pancreas, brings that sugar into your cells, where it’s used for energy. If your body can’t properly use its insulin or doesn’t make enough (which is what happens when you have diabetes), sugar builds up in the bloodstream.
That direct link between food and glucose—between nutrition and diabetes—is what makes what you consume important. By tapping into how you eat, you may notice an impact on blood sugar levels and how you feel.
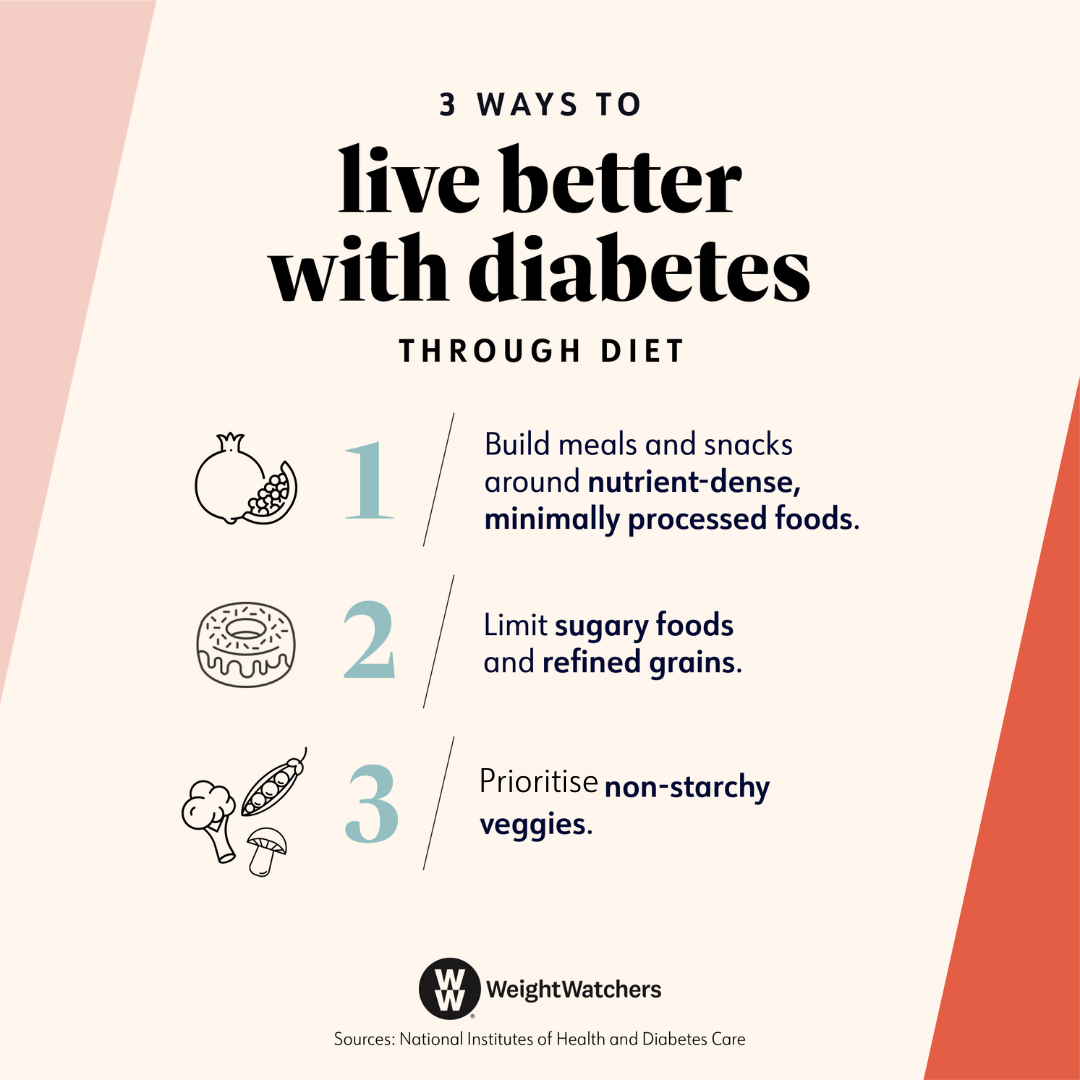
Dietary recommendations for diabetes
Nothing is completely off-limits, but there are a few foods that get a gold star for people living with diabetes. You can follow these general principles the next time you’re grocery shopping.
- Fibre-rich carbs. Oats, brown rice, quinoa, wholegrain bread, and whole-wheat pasta are great grain choices because they’re high in fibre, which is something people with diabetes should prioritise. Research shows that increasing your fibre intake is tied to better blood sugar control. "Fibre slows the breakdown of carbohydrates in the body," says Courtney Wilson, R.D., a registered dietitian and a certified diabetes care and education specialist at Texas Health Resources, in Texas, United States. "This allows glucose to slowly enter the bloodstream, giving the body time to process it and not cause a blood sugar spike."
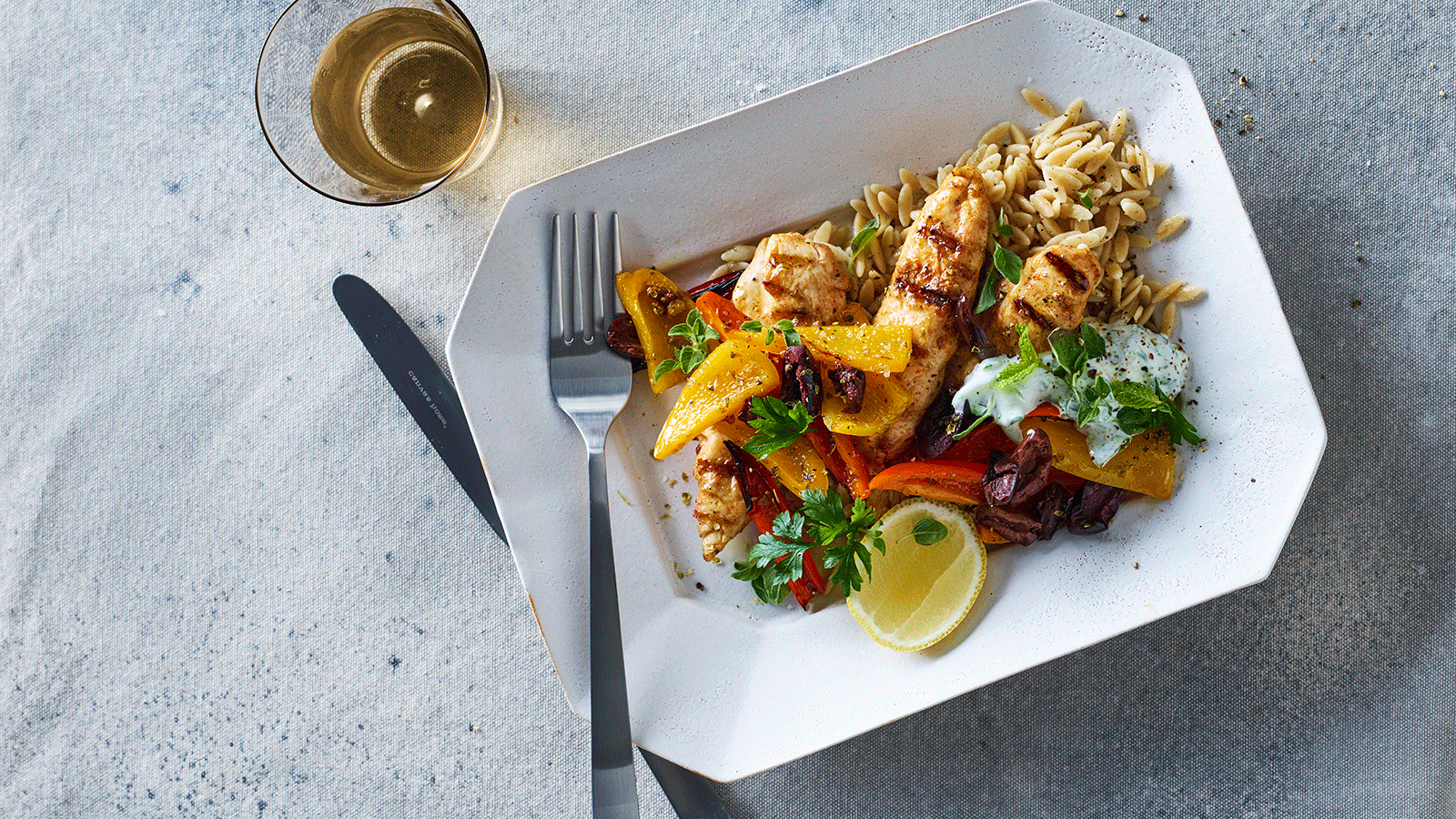
- Lean sources of protein. Skinless chicken, fish, shellfish, eggs, tofu, and legumes help you feel full without having a large impact on blood sugar. Aim to include one type of lean protein with each meal or snack. "Have a scrambled egg with a bowl of polenta, or enjoy lean turkey and cheese with a sliced apple," says Angela Ginn-Meadow, R.D., a registered dietitian, a certified diabetes educator, and the senior diabetes educator coordinator at the University of Maryland Medical Center in Baltimore, United States.
- Heart-healthy fats. Unsaturated fats—found in olive oil, canola oil, avocados, or nuts—can support heart health. The opposite holds true for saturated fats, which are found in foods like meat, full-fat dairy, and tropical oils and can build up in your arteries and lead to high cholesterol. Diabetes increases your risk of heart disease.
Still not sure what to eat on a daily basis with diabetes? Accredited Practising Dietitians (APDs) and diabetes educators who specialise in the management of diabetes can help you find a diet that fits your lifestyle and addresses your individual concerns. Your doctor should be able to give you a reference for someone who can help.
Foods you should avoid for diabetes
No food should be entirely off-limits. Being able to enjoy the things you love is key for making your eating plan sustainable so you can better control your diabetes long-term, says Vandana Sheth, RDN, a registered dietitian nutritionist and a certified diabetes care and education specialist in Los Angeles, United States.
However, certain foods, like the ones listed below, can make it harder to manage your blood sugar, raising your risks of diabetes-related complications, like high blood pressure or heart disease. You can still eat the following, but it's best to indulge occasionally and in smaller portions.
- Refined grains, like white bread, white pasta, or white rice
- Sweets and desserts, including baked goods, ice cream, and lollies
- Fried foods
- Foods high in saturated fats, such as fatty or processed meats, full-fat dairy, and coconut and palm oils
- Shortening
- Foods high in sodium, like processed snacks
- Drinks with added sugars, including soft drinks, juice, sweetened teas, sports drinks, and energy drinks
- Alcohol (if you choose to drink it), particularly if you take insulin or diabetes medications
Finding a good diet for diabetes
Coming up with the perfect diabetes diet is tricky because no two people are alike. The best foods to eat, along with how much to eat and when, depend heavily on things like the type of diabetes you have, how much activity you do each day, and whether or not you’re on medications, says Sheth.
Looking for a more specific plan to follow? Many of the most popular ones out there, including the WeightWatchers® diabetes program, fit within the above guidelines. The right approach for you: Choose a way of eating that makes you feel good and is easy to stick with. Here are some techniques to consider talking about with your doctor, dietitian or nutritionist.
1. Diabetes plate method
You know those divided plates used for little kids? That’s the idea with the diabetes plate method—except this time, you’re drawing imaginary lines that divide your plate into four equal sections.
- Fill two of the sections, or half your plate, with non-starchy vegetables. These are all those veggies that are a colour of the rainbow: broccoli, carrots, cauliflower, capsicums, asparagus, and salad greens.
- Fill one-quarter of your plate with lean protein. Chicken (skinless), turkey, eggs, and seafood work, as do lean cuts of beef or pork. Don't forget plant-based protein sources (like legumes and tofu)—they count too.
- Fill one-quarter of your plate with carbohydrates. These include wholegrains, starchy vegetables (like potatoes, sweet potatoes, butternut pumpkin, or corn), fresh fruit or dried fruit, and dairy foods.
- Add a glass of water. Sip on something like sparkling water or unsweetened iced tea.
Pay attention to your plate size too. For meals, this method recommends using a 23 cm(or nine-inch) plate, which holds enough food to fill you up but not so much that you end up overeating. As for snacks, choose ones that are high in fibre, protein, or healthy fats to keep you feeling satisfied between meals.
It’s OK if you don’t hit the mark for every single meal. For example, you might find it hard to eat vegetables, protein, and carbs at breakfast if you don’t wake up super hungry. In that case, try to have at least two of those food categories and include plenty of filling fibre and protein. (One easy option: scrambled eggs with berries on the side.)
2. Mediterranean diet
Inspired by the traditional eating habits of people in Greece, Italy, and Spain (where many chronic conditions are rare), the Mediterranean diet has been shown to support heart health and lower the risk of type 2 diabetes. Researchers have also found that it can decrease blood sugar levels in people with diabetes. The benefits are thought to come from the diet's anti-inflammatory and antioxidant effects and its ability to support healthy gut bacteria.
Here’s what the Mediterranean diet tends to look like.
- An emphasis on plant-based foods (like wholegrains, vegetables, legumes, fruit, nuts, seeds, herbs, and spices)
- Healthy fats (like olive oil) typically used instead of butter
- Animal foods (like fish, dairy, and eggs) eaten in moderation
- Red meat and sweets consumed less often
- Fresh fruit often served for dessert
Alcohol in moderation, particularly red wine, can be a part of a Mediterranean-style diet too. But it’s worth noting that drinking too much (especially on an empty stomach) can lead to low blood sugar.
3. DASH diet
DASH, or dietary approaches to stop hypertension, was created to help lower high blood pressure, which affects two out of three people with diabetes. But it can also help manage diabetes by improving insulin resistance, lowering cholesterol, and supporting a healthy weight.
The DASH diet encourages people to eat foods that are minimally processed and low in saturated fats, like wholegrains, fat-free or low-fat dairy products, fruit, vegetables, poultry, fish, and nuts. Fatty meats, full-fat dairy products, tropical oils (like coconut or palm), sweets, and sugary beverages aren't entirely off-limits, but they should be enjoyed sparingly.
How much you can eat is based on your daily recommended calorie (a.k.a. kilojoules) intake. But to give you an idea, here’s what someone eating 1,600 calories would consume on the DASH diet.
- Six servings of grains (at least half should be wholegrains)
- Three to four servings of vegetables
- Four servings of fruit
- Two to three servings of dairy
- 170g or less of meat
- Three servings of nuts, seeds, or legumes per week
4. Plant-based diet
One of the trendiest eating plans these days, a plant-based diet consists mostly of, you guessed it, plant foods. This includes wholegrains, fruit, vegetables, legumes, nuts, and seeds. Following a healthy plant-based eating plan is associated with a lower risk of developing type 2 diabetes, likely due to its ability to reduce insulin resistance, promote a healthy body weight, and support a balanced gut microbiome.
There’s a whole spectrum of approaches to plant-based diets, from flexitarian (where you can eat some meat, seafood, and poultry, but only occasionally and in small quantities) to vegan (where you completely avoid all animal products, including meat, seafood, poultry, eggs, and dairy).
5. WeightWatchers diabetes program
Rather than overhauling your entire diet, WW’s plan for diabetes helps you tweak the way you eat to help you lose weight and support healthy blood sugar levels. Every day, you get a set amount of Points, which represent a food’s nutritional value.
“The plan's ZeroPoint foods list is tailored to include foods that are mostly lower in carbohydrates—things like non-starchy vegetables and lean proteins encourage members to reach for them often,” says Angela Goscilo, M.S., R.D. “The Points algorithm also raises the Points value of a food that is higher in added sugars, nudging members toward foods that are lower in added sugars.”
Research found that on average, after six months, participants on the WeightWatchers diabetes program lost 5.17% of their weight and reduced their HbA1c levels by 0.76 percentage points.*
Tell me more about…
low blood sugar
Q: Is low blood sugar dangerous?
A: As much as you may focus on blood sugar getting too high, you also don’t want it to drop too low since it’s an essential source of energy for our cells and muscles. “Low blood sugar, or hypoglycaemia, can occur in people taking medication for diabetes and, in particular, when taking insulin,” says Dr. Ari Geliebter, M.D., the chief of endocrinology at Holy Name Medical Center, in New Jersey, United States. Defined as a blood sugar level of less than 70 mg/dl (milligrams per deciliter), prolonged hypoglycaemia can result in seizures, coma, and, in some rare cases, death.
Q: What are the symptoms of low blood sugar?
A: “They vary from person to person, but early signs tend to include fatigue, dizziness, sweating, hunger, tingling lips, a fast or pounding heartbeat, and pale-looking skin,” says Geliebter. If your blood sugar stays low for a while, you might start to get more serious symptoms, such as feeling weak, losing your concentration, having blurred vision, or feeling sleepy.
Q: Is it possible to have low blood sugar and not even know it?
A: Yes, it’s called hypoglycaemia unawareness, and it occurs after you’ve had several episodes of low blood sugar. When your brain and body become so used to having too-low levels of glucose in your blood, they stop sending you messages that something is wrong (which you would experience through common symptoms of diabetes). “This can be dangerous, as it might lead you to go too long before increasing your blood sugar levels,” says Geliebter.
Hypoglycaemia unawareness is one reason why it’s important to follow your doctor’s advice on how often to get your HbA1c level checked. This tests your average blood sugar levels over the last few months. The results can help make sure you’re managing your diabetes correctly. You might also benefit from a continuous glucose monitor, which will alert you if your blood sugar levels get too low.
Q: What’s the quickest way to get low blood sugar back up?
A: The quickest way to treat low blood sugar is to eat or drink something with fast-acting sugars, such as fruit juice, glucose tablets (available at the pharmacy), or hard lollies, says Geliebeter. Consume at least 15 grams of carbohydrates right away, then wait 15 minutes to see if you feel any better.
Eating sugar if you have diabetes
There’s no reason to avoid sugar completely if you have diabetes, but you’ll want to keep an eye on portion sizes since foods with added sugars can have a big impact on blood sugar, making it harder to stick within your target range. You can help minimise this by pairing a dessert with protein or fibre. This slows the rate at which the sugar is absorbed into your bloodstream and reduces blood sugar spikes, Sheth says. You can get a similar effect by having a treat immediately following the end of the meal, as opposed to alone as a snack.
Being active after eating something sugary can also be helpful. "I often advise my clients to consume sweets with meals and go for a walk afterward," Ginn-Meadow says. Physical activity within 30 minutes of eating can lower blood sugar levels, since your muscles use some of the sugar you've eaten for fuel.
The connection between carbohydrates and blood sugar management
Paying attention to your carbohydrate intake is important. Eating too many carbs at once can cause excess glucose to build up in your bloodstream while not eating enough can lead to low blood sugar. Both high and low blood sugar can make it harder to manage your diabetes and increase your risks of complications over time.
But it’s not just total carbs you should care about; you also want to make sure you’re getting carbs from the right sources. Complex or high-fibre carbohydrates, like wholegrains and legumes, have less of an impact on blood sugar than sugary or refined carbs, like biscuits, white pasta, or potatoes. That makes them a healthier choice for people with diabetes.
The way carbs are spread throughout your day matters too. (You don’t want to eat an entire day’s worth in one sitting.) An accredited practising dietitian or a diabetes educator can help you determine the amount of carbohydrates to consume during a meal or snack. "Some people may be able to enjoy a sandwich on two slices of wholemeal bread, for instance, while others may be able to add a medium-size piece of fruit," Sheth says. And if you take insulin, you'll need to count exactly how many grams of carbs you consume in a meal or snack, since that will help you determine how much insulin you need to take.
Possible increased risks of certain vitamin or mineral deficiencies
Changing your diet plus eating a different mix of foods plus taking different medications can have an impact on vitamin and mineral levels. For example, taking the prescription diabetes medication metformin can lead to low levels of vitamin B12. (Nearly a third of people who take the drug are deficient.) Since B12 is involved in healthy nerve function, getting the recommended amount may reduce pain related to nerve problems, like diabetic neuropathy. If you are concerned about vitamin and mineral levels, talk to your doctor about a blood test to assess your specific needs.
The relationship between diabetes and nutrition is a complicated one, so when in doubt, talk about it with your doctor or dietitian. They will be able to help you make informed decisions, whether it’s determining the right amount of carbohydrates to eat, choosing an eating plan to follow, or figuring out if you need to supplement any nutrients.
This content is for informational purposes only and does not constitute medical advice, diagnosis or treatment. It should not be regarded as a substitute for guidance from your healthcare provider.
*Based on a six-month single-arm multicenter trial that tested the WW Diabetes Program and was led by John Apolzan at the Pennington Biomedical Research Center from April to December 2021.
