BMI Calculator | Check your BMI | WW UK - WeightWatchers
BMI calculator
Use our BMI calculator to check your body mass index (BMI) and find out if you're a healthy weight.

Understanding your BMI result
Under 18.5
Underweight. This could be a sign that you're not eating enough, or indicate underlying medical conditions. Your GP can help if you're underweight.
18.5 – 24.9
Healthy weight. Keep up the good work!
25 – 29.9
Overweight. Building healthy habits, like eating healthily and being more active, can help you lose weight.
30+
Obese. Losing weight and working towards a healthy BMI should be a priority. Your GP can support you with this.
My BMI is too high, what can I do to lose weight?
A good initial goal to aim for is losing 10% per cent of your body weight. Even if that’s not enough to push you into a healthy weight range, it’s a great start when you’re overweight, with research showing it’s enough to deliver health benefits, like lowering risk factors for type 2 diabetes and heart disease. The WeightWatchers® programme encourages members to focus on realistic weight-loss goals and provides the skills and techniques to help you achieve them.
How to maintain a healthy BMI
There are lots of small steps you can take to maintain a healthy BMI, including small changes to what you eat, how you exercise, and your daily habits, such as:
A healthy balanced diet
Make sure your diet has a good mix of fruit, vegetables, starchy foods, and proteins, with a smaller amount of high fat or high sugar foods.
Monitoring portion sizes
Keep an eye on your portion sizes if you notice your BMI starting to creep up. Weighing out your foods and tracking your meals can help with this.
Staying active
Not only can regular exercise help maintain a healthy weight, it can also reduce your risk of major illness and keep your mental wellbeing in check.
Cutting down on alcohol
Current NHS guidelines state both men and women should not exceed more than 14 units of alcohol per week.
Our customised weight loss plans can help lower your BMI.
What is BMI and what does it measure?
BMI - otherwise known as body mass index - is a simple measure of weight in relation to height. It estimates percentage of body fat, and is used to broadly determine if you’re a healthy weight for your height.
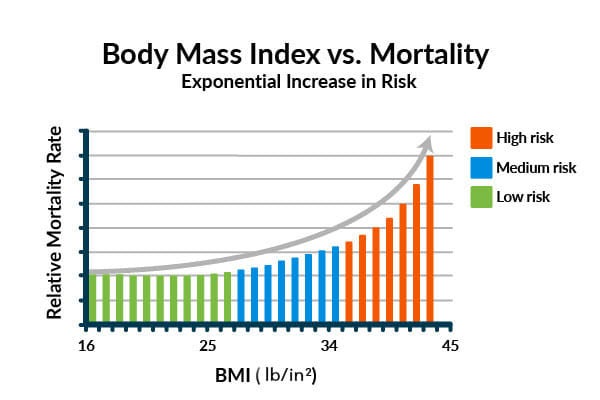
A higher percentage of body fat is proven to be associated with increased risk for developing certain diseases such as heart disease, high blood pressure, type 2 diabetes, breathing problems, cancers and a higher risk of early death.
Being underweight may indicate underlying medical conditions or an eating disorder, plus higher risk for conditions such as osteoporosis.
You can use the BMI calculator at the top of this page to work out the BMI for you and the adults in your family.
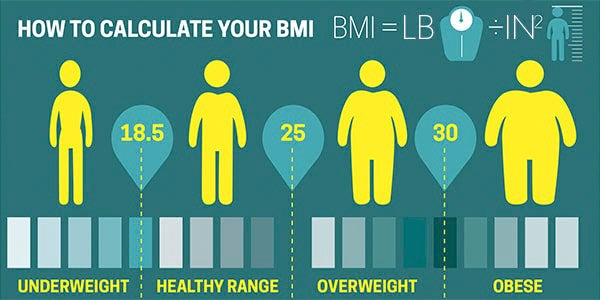
How to calculate your BMI
BMI is a simple calculation using a person’s height and weight. The formula is BMI = lb/in2 where lb is a person’s weight in pounds and in2 is their height in inches squared. Enter your weight and height into our BMI calculator to find your result.
What is a healthy BMI?
For most adults, an ideal BMI is in the 18.5 to 24.9 range.
Is BMI more important for women or men?
The same BMI measurements apply to both genders as the same risks of developing weight-related illness applies to both women and men.
Research has made the connection between having a higher BMI and an increased risk of a number of diseases, including heart disease, type 2 diabetes, osteoarthritis and certain types of cancer including breast cancer.

Is BMI reliable?
BMI is a very simple measurement. While it takes height into consideration, it does not account for factors such as waist or hip measurements, proportion or distribution of fat, or proportion of muscle mass. BMI results may be a less reliable indicator of health for certain demographics, including:
Older people
Because muscle mass tends to drop and body fat tends to rise in older people, BMI may not be an accurate reflector of body fat if you're over 60.
Athletes and people with lots of muscle
People who carry a lot of muscle but little fat (such as bodybuilders and athletes including boxers and rugby players) may fall into the ‘overweight’ or ‘obese’ category when calculating their BMI - despite the fact that they may be fit and healthy.
Pregnant women
You should have your BMI calculated at your first antenatal booking appointment. If you have a BMI of 30 or above, your midwife should give you information about the additional risks as well as how these can be minimised and about any additional care you may need.
People less than 5 foot tall
The BMI calculation isn’t always accurate for people under 5 foot tall, who might be shown a ‘healthy’ result even if they are carrying too much body fat.
Children and teenagers
This BMI calculator has been designed to calculate the body mass index of adults. Please see your GP if you’re concerned about your child’s weight.
Some ethnic groups
Black, Asian and other minority ethnic groups with a BMI of 23 or more have a higher risk of getting type 2 diabetes and other long term illnesses.
Should I bother calculating my BMI?
Yes, says Dr Michelle Celander, WW program and Science Director. “BMI provides a snapshot of how weight affects the risk of medical problems for a population of people, so while it may not be a perfect measure of medical risk for every individual, it’s still very valuable as feedback for you.
“But, while it is a good idea to calculate and know what your BMI is, no one piece of feedback about your weight or health should be viewed in isolation, so it’s really
What to do if you’re worried about your BMI
If our BMI calculator finds that your BMI is outside of the healthy range, we recommend you talk to your doctor before making any big changes. However, there are some small steps you can take towards a healthier lifestyle to achieve your weight loss goals. Browse our Recipes page for delicious, healthy meals and get expert advice on everything from exercise to sleep in our Healthy Living Hub.
How to lower your BMI with WW
Stepping on the scales may seem daunting, but once you know your weight, you’re in a good place to make an action plan for success. The Points® programme offers a safe and sustainable way to lose weight, at a rate of around 1-2lb per week, without having to count calories or go hungry. You can choose from two different plans - Core and Premium membership. Each one offers something a bit different, so there’s bound to be one that fits in with your lifestyle.
Dishes to help keep your BMI in the healthy range
BMI Frequently Asked Questions
The BMI scale is the same for both men and women. It takes into account a person’s height and weight.
BMI is a simple calculation using a person’s height and weight. The formula is BMI = lb/in2 where kg is a person’s weight in pounds and in2 is their height in inches squared. Enter your weight and height into our BMI calculator to find your result.
For most adults, at most ages, an ideal BMI is in the 18.5 to 24.9 range.
YES
A BMI of 18.5–24.9 is considered “normal” weight with a low risk of poor health, while anything above or below may indicate a higher risk of poor health.